A new therapy developed by U of T Scarborough researchers may bring us one step closer to effectively killing deadly drug-resistant 'super-bugs.'
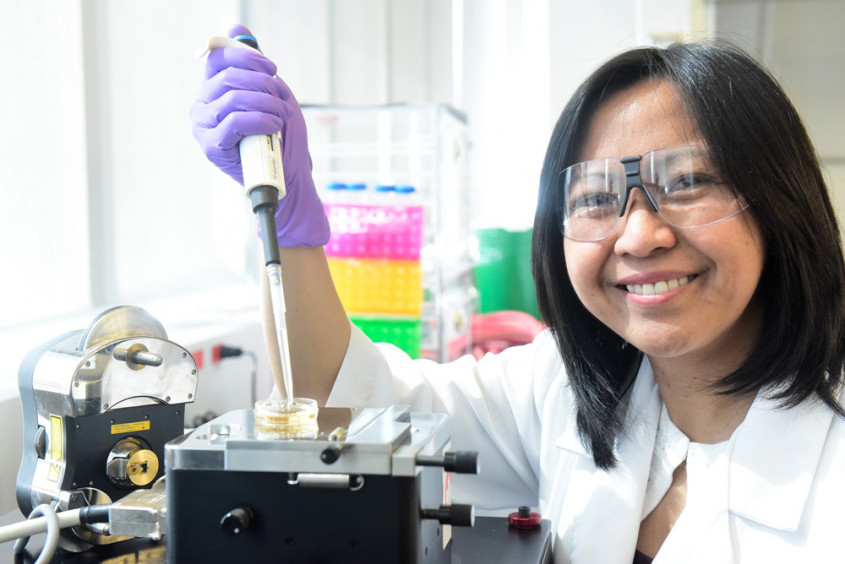
“The threat posed by pathogens that are increasingly becoming resistant to all known antibiotics is an alarming and pressing health care problem,” says Ruby Sullan, assistant professor in the department of physical and environmental sciences at U of T Scarborough.
“It’s resulting in hundreds of thousands of deaths and billions of dollars in health care costs annually, so there’s an urgent need to seek alternatives to antibiotic-only therapies.”
The therapy developed by Sullan and post-doctoral researcher Nesha Andoy, uses nanoparticles made from polydopamine, a naturally occurring hormone and neurotransmitter, making it highly compatible with the human body.
The therapy can kill bacteria in two ways. The surface of the nanoparticles are coated with an antimicrobial peptide (AMP) that targets and kills the bacteria by binding to and destabilizing its membranes. Since the dopamine-based particles are also highly photosensitive, they are able to heat up when exposed to low-powered laser light, killing the bacteria through heat.
Sullan says a major benefit of using these nanoparticles is that it allows the bacteria to be killed at a lower temperature using lasers, leaving the surrounding healthy cells unharmed.
“Since the mechanisms that this therapy uses is different from most antibiotics, we envision that they can be designed and developed to target other drug-resistant bacteria,” she says.
Antimicrobial resistance (AMR) happens when bacteria or fungi evolve to become immune to antibiotic drugs. While Sullan and her team tested this therapy on E.coli as part of the research – some strains of which can cause serious health problems in humans – it may eventually be used to kill a range of drug-resistant pathogens, including the bacteria that result in hospital staph infections.
If it sounds reminiscent of cancer therapies, it should. Sullan says they drew inspiration from polydopamine, which is widely studied for cancer therapy.
“Polydopamine is a well-studied nanomaterial for anti-tumor applications, but our twist is that we used it to target infection caused by bacteria,” she says.
Sullan is quick to note that this therapy doesn’t completely eliminate bacterial-resistance, which is likely impossible to do. After all, bacteria were among the first life forms on earth, can be found living in the most extreme environments, and will likely survive long after we’re gone.
“The technology we’ve developed is designed to curb the onset in which bacteria resistance develops,” says Sullan, whose research explores bacterial adhesion.
“If we can confuse the bacteria by killing it several different ways, it will have difficulty evolving quickly enough to develop resistance to these different types of mechanisms that can kill it.”
The research, which is published in the journal Advanced Functional Materials, received funding from the Canada Foundation for Innovation (CFI), Natural Science and Engineering Research Council of Canada (NSERC), Ontario Ministry of Research, Innovation, and Science, U of T Connaught Fund, and U of T Scarborough Research Competitiveness Fund.
Sullan’s lab is currently looking at ways to decrease the size of the nanoparticle to make it more suitable for use in living organisms, and exploring ways to improve its efficiency. Since the system they’ve developed is highly modular, she says it can be modified to change its killing mechanisms, like changing the coating to different antimicrobial agents or loading it with antibiotic drugs.
“That could make a third bacteria-killing mechanism, so it would really enhance it as a multi-functional therapy for drug-resistant pathogens.”
